Maggie post op in recovery
When Maggie’s mum noticed she wasn’t eating and slept in longer than usual one Sunday morning, she knew something was wrong and brought her in to VS A&E. Maggie is no stranger to us at VSA and we know how much she loves food, so even though she looked fine on the outside, her history of dietary indiscretion, oesophageal foreign bodies, ureteral obstructions and chronic kidney disease had us wondering what was happening inside. Little did we know at the time she would become a very complex case.
Dr Dinindu Jayasuriya examined Maggie, performed blood tests and looked at her abdomen and bladder briefly on ultrasound to check there were no obvious foreign bodies or obstructions. Maggie’s blood results showed elevated kidney values, so she was started on pain relief and fluids.
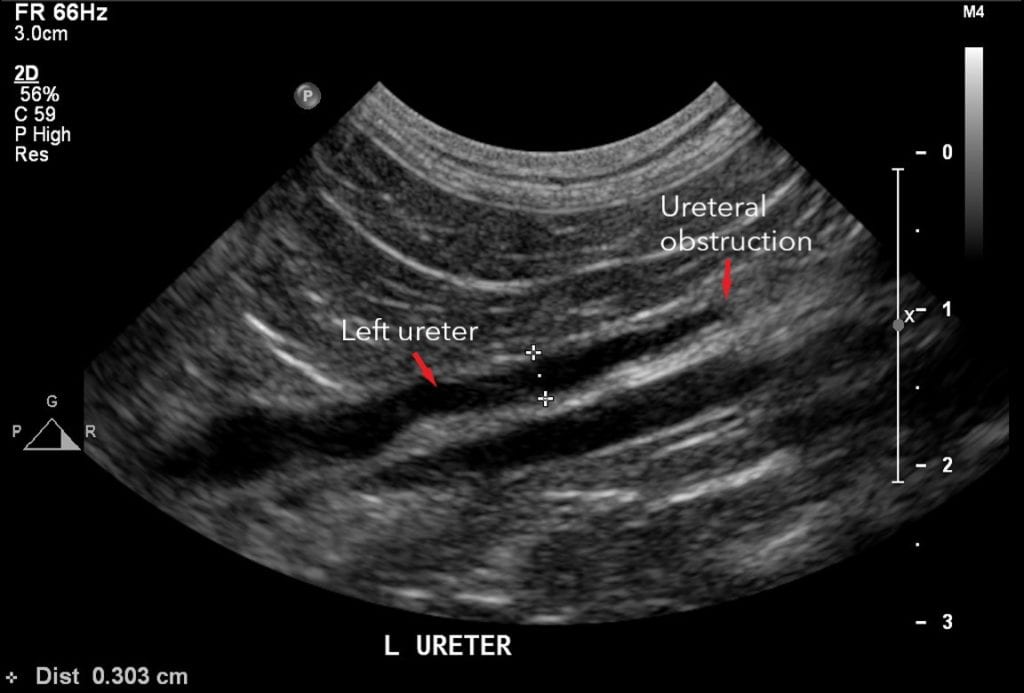
The following morning, Maggie was transferred to Internal Medicine Specialist, Dr Mike Coleman who performed a comprehensive ultrasound which showed an obstruction in her right ureter (the tube carrying urine from the kidneys to the urinary bladder). Dr Coleman started Maggie on medications to help relax the ureter and increase urine production to assist moving the stone, while also continuing pain relief and IV fluid therapy.
By Tuesday morning, less than 24 hours after beginning the prazosin, Maggie appeared to be having an adverse reaction – she was very flat and lethargic, and excessively drooling, so the prazosin and mannitol were stopped. A repeat abdominal ultrasound was performed which showed some improvement in her right kidney, but changes were now being noticed in her stomach. Dr Coleman consulted with Specialist Surgeon, Dr Alastair Coomer who recommended continuing the current medical management plan and continuing with serial ultrasounds to monitor the progression of the obstruction.
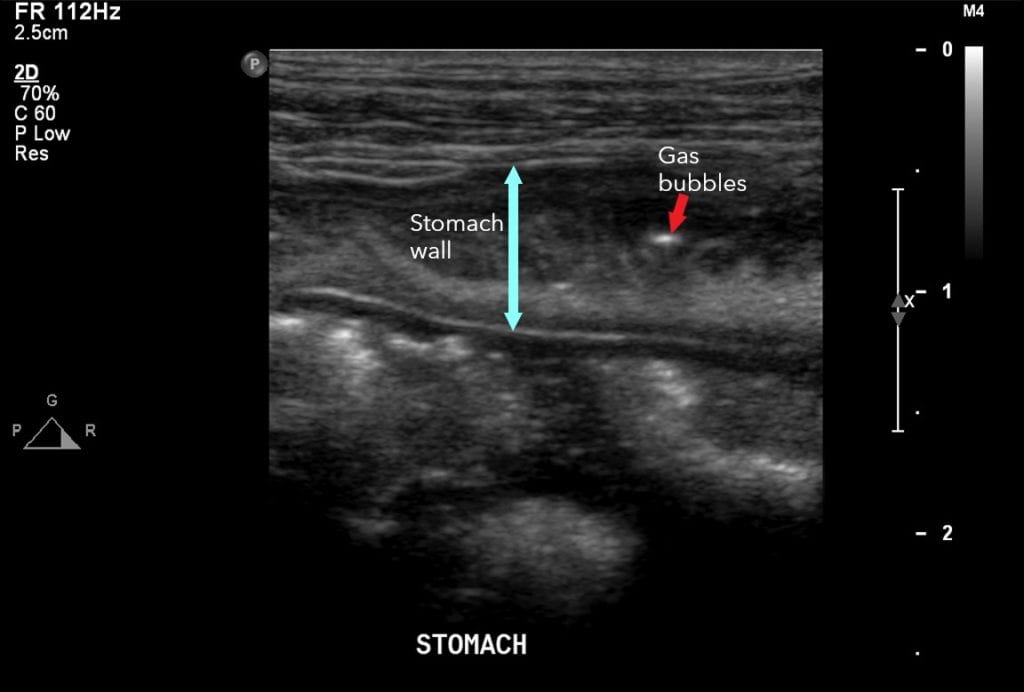
Maggie was transferred to our Mt Albert hospital on the Thursday where she had another ultrasound with Specialist Radiologist, Dr Ben Wernham. Following the ultrasound, the main concern was no longer her ureter, but her stomach – those changes that were beginning to be noticed were now our biggest concern. Dr Wernham observed on ultrasound that Maggie’s stomach wall was severely thickened, had loss of normal stomach wall layering and had multiple pockets of gas scattered throughout the stomach wall. These findings indicated Maggie had severe emphysematous gastritis. Emphysematous gastritis is a rare and potentially fatal condition that has only been reported in 2 other feline cases with none of our specialist vets, who collectively have over 100 years of experience, ever seeing something like this before.
Dr Tommy Fluen from Veterinary Internal Medicine Specialists and his team immediately performed a gastroscopy to evaluate what was happening inside her stomach. Her stomach lining was black, indicating necrosis, and she needed to go straight to surgery to check that it had not progressed through the entire stomach wall. Dr Alex Walker performed a full thickness biopsy (taking a 1cm biopsy) of the stomach wall and was able to observe that the necrosis had only affected the lining of the stomach. Dr Walker also placed an oesophageal feeding tube to ensure nutritional support for her stomach’s recovery and to be able to give her oral medications. Maggie was immediately started on triple antibiotics as it was unclear what had caused the infection. The histopathology results of the stomach biopsy returned as pasteurella multocida – a bacteria that commonly lives in the mouth but had just gone crazy in Maggie!
Following a day’s rest and monitoring for Maggie with our nursing team and a feeding tube tutorial for Maggie’s mum and dad with nurse Gerry, she was discharged on the Saturday. Unfortunately, her story didn’t end there.

Maggie had been at home for a week and all was going well until she began frothing at the mouth and became lethargic. She returned to VS A&E where she saw Dr Izzy MacEwan. As Maggie has quite a low tolerance to medication, Dr MacEwan suspected she may have had an adverse reaction to an appetite stimulant she was given the day before and admitted her for IV fluid therapy and pain relief.
Dr Coleman examined Maggie on the Monday morning and performed another ultrasound. The news was not good, Maggie now had a left ureteral obstruction. We continued IV fluids and low dose pain relief, along with daily serial ultrasounds to monitor the progression of the obstruction.
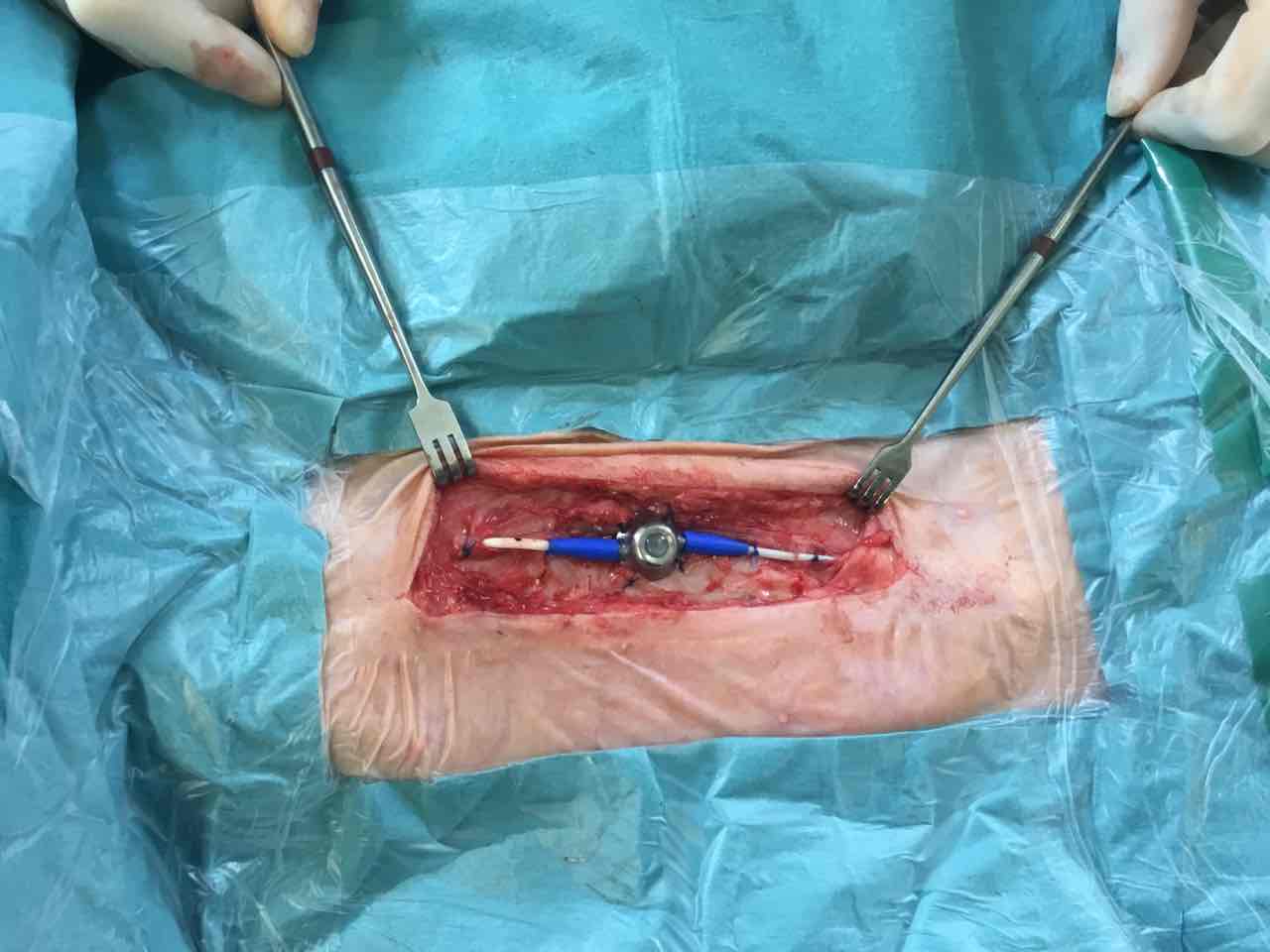
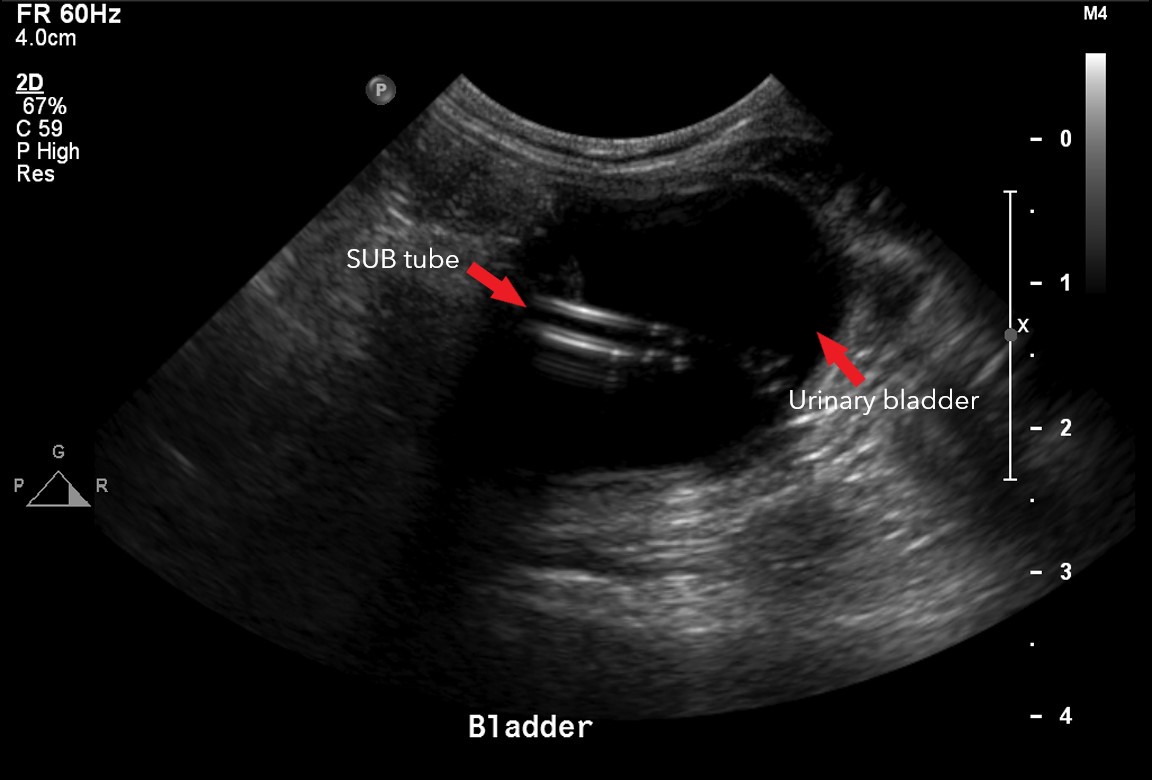
By Thursday, Dr Coomer had a long discussion with Maggie’s mum about surgical intervention, namely the placement of a subcutaneous ureteral bypass (SUB) device where a tube is inserted into the kidney and connected to a port which sits just below the skin, where a second tube is connected that is inserted into the bladder. This effectively creates a false ureter.
As Maggie was still recovering from surgery, the decision was made to continue with medical management to see if the obstruction would pass. Our VS A&E team continued to monitor her over the weekend with lots of cuddles and visits from her family.
The following week, Dr Coomer made the decision to take Maggie to surgery and place a SUB as the obstruction was not going to budge. At her mum’s request, Maggie was given a cool haircut as the last thing she needed at this point was an obstructed hairball!
Maggie had a consultation the following day with visiting Cardiologist, Dr Jacqui Huxley of Apex Cardiology, due to a transient heart murmur observed. Dr Huxley had a few tricks up her sleeve and Maggie was very settled in her procedures with her and didn’t require any sedation which none of our nurses believed! Thankfully, Maggie was given the all clear by Dr Huxley.
Maggie recovered well and was able to go home that weekend. She was even eating well and able to have her feed tube out the following Monday. Her repeat blood work the following week looked fantastic with everything in normal range.
SUB surgery requires a lifelong commitment with the device needing to be flushed every 3 months and blood work every 6 months. The device also needs to be flushed in the first 2 weeks after surgery to check that it is functioning correctly. Maggie, not being one to do things the easy way, needed a third surgery to have a slight adjustment to her SUB.
Maggie spent a total of 3 weeks in hospital, saw 6 specialists and had the involvement of more than 50 nurses and emergency vets across 2 hospitals.
One year on, Maggie continues to do well and has regular, routine monitoring with us for her SUB.



